What is Erb’s Palsy?
Erb’s Palsy is a birth injury in which nerves at the base of the baby’s neck are damaged during delivery resulting in full or partial paralysis in the baby’s arm. Children with Erb’s Palsy (or Erb-Duchenne Palsy) will have some level of physical disability and paralysis in the affected arm. The most severe cases of Erb’s Palsy can involve complete paralysis from the shoulder down, but most cases involve only moderate immobility.
Erb’s Palsy is an injury during childbirth, not a disease. It results when a baby’s brachial plexus nerves are torn during a difficult vaginal delivery. Like other birth injuries, Erb’s Palsy can be prevented with proper obstetric care. OB/GYNs should recognize the risks factors for nerve damage and Erb’s Palsy and take preventive measures.
Medical Definition of Erb’s Palsy
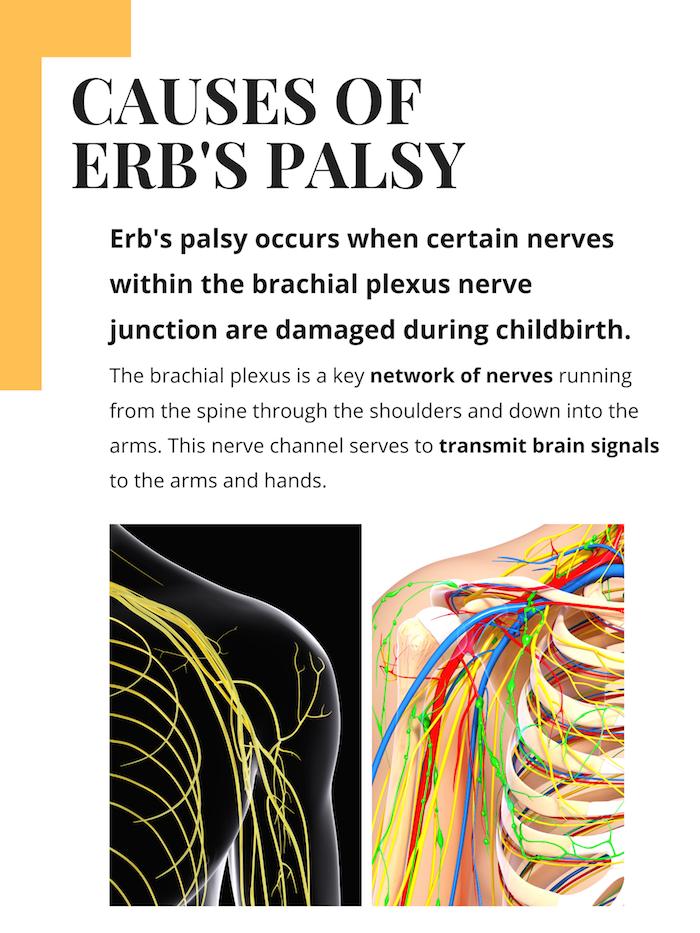
The brachial plexus is cluster of nerves in the shoulder area which connects the neck to the arm. Erb’s Palsy is defined as arm paralysis caused by injury to a specific merger point of 2 nerve roots (know as “Erb’s point”) in the brachial plexus. Erb’s Palsy can be distinguished from other types of brachial plexus injuries (such as Klumpke’s Palsy) based on the location of the nerve injury. Erb’s Palsy specifically affects the upper two of the five brachial plexus nerves (C5&C6) and often does not prevent lower arm movements such as the wiggling of fingers.
Klumpke’s Palsy is similar but less common and it happens when the nerve damage occurs in a different junction point in the brachial plexus. Klumpke’s Palsy involves injury to the lower nerve junctions (the C8 and T1 nerve roots).
The brachial plexus is the most important set of nerves located within the arm, and their role is to give movement, flexibility, and feeling to the arm, hand, and fingers. These nerves consist of thousands of fibers that carry electrical signals back and forth between the brain and the muscles of the arm and hand. When injured, normal nerve impulses are impaired and the spinal cord is unable to send messages to the arm, hand, wrist, and/or fingers as they normally would.
Presentation and Characteristics of Erb’s Palsy
The singular characteristic of Erb’s Palsy is immobility, weakness, or paralysis in the arm. Paralysis is from the shoulder down and can be complete or only partial. Feeling and sensation is usually diminished in the arm. This lack of sensation, combined with the paralysis, usually leads to muscular atrophy in the biceps, deltoid, and other arm muscles.
In moderate to severe cases of Erb’s Palsy, the affected arm will often be noticeably abnormal in physical appearance. The arm will hang awkwardly and rotate inward. The atrophy of the biceps causes the wrist to be pulled or flexed instead of straight. This is sometimes described as “waiter’s tip arm” because it looks similar to a waiter when receiving a tip. The impacted arm will often have stunted growth and be noticeably smaller than the other arm.
Categories of Erb’s Palsy
Depending on the severity of the injury, Erb’s Palsy is typically classified into four categories, which are characterized as follows:
- Neuropraxia – As the mildest form of Erb’s Palsy, the brachial plexus is stretched or shocked but does not tear. This is the easiest form to deal with, and also the most common. Although it typically heals completely within three months, it can still send burning pain and your child may experience some intense discomfort during this time.
- Neuroma – This is a consequence of more serious stretching, in which some nerve fibers have also been damaged. As a result, this can lead to scarring and discomfort, and long-term recovery is usually partial. It is accompanied by the same burning sensations as neuropraxia and should heal – but not always fully. Physical therapy and surgery typically help with the recovery.
- Rupture – This is a stretch injury from nerve tearing, and requires surgery to repair the nerve – it can’t heal on its own. This is usually done by a physician who splices and grafts a healthy nerve from another part of the body, which will return feeling, flexibility and support to the affected area – but there will be challenges even after treatment.
- Avulsions – As the most severe form of Erb’s Palsy, the nerve has been totally torn from the spinal cord. Your child’s arm will be completely motionless but may be able to regain its mobility after surgery. Some recovery is possible but typically only with surgical intervention.
Erb’s Palsy Treatment Options
Treatment options for Erb’s palsy vary depending on the nature and severity of the condition in each individual case. For less severe cases, treatment is usually limited to various types of therapy. The more serious cases will often require surgical treatment in addition to therapy.
Hydrotherapy: Hydrotherapy is essentially physical therapy done underwater. The low-gravity environment creates less stress on the infant’s body and allows more freedom of movement. The goal of hydrotherapy is to strengthen the muscles and eliminate spasms. The hydrotherapy program will usually involve abduction of the shoulder, supination of the forearm, and shoulder rotations.
Physiotherapy: Physiotherapy can be performed on its own or alongside hydrotherapy. The effectiveness of the therapy varies among patients; some may recover more quickly than others. In severe cases, physical therapy might be necessary to complement surgery, while in milder conditions, it can help strengthen the affected area and promote self-healing. Different types of physical therapy exercises may include gentle stretching, sensory stimulation, range-of-motion exercises, and strength training.
Surgery: Surgical treatment options for Erb’s palsy are usually reserved for only the most severe cases where treatment with physiotherapy or hydrotherapy is not effective. The most common and most effective surgical treatment option is a nerve graft procedure that attempts to rebuild the damaged nerves that cause Erb’s palsy. Another surgical option is nerve decompression surgery, although this has a lower success rate.
Current Research on Erb’s Palsy
- Ahmed, Mona Mohamed Ali, et al. “Effect of Mirror Therapy on Fine Manual Control in Children with Erb’s Palsy.” Egyptian Journal of Hospital Medicine 92.1 (2023). This study examines the effectiveness of “mirror therapy” on children with Erb’s palsy. It concludes that mirror therapy can be helpful in improving outcomes, but only when combined with traditional therapy methods.
- Spiegel, Efrat, et al. “Obstetric risk factors for severity of Erb’s palsy.” American Journal of Obstetrics & Gynecology 228.1 (2023): S296. THe most recent comprehensive study on the obstetric risk factors for Erb’s palsy. The connection between specific obstetric risk factors and Erb’s palsy was assessed based on an analysis of data over a 10-year period.
- Yarfi, C., Elekusi, C., Banson, A. N., Angmorterh, S. K., Kortei, N. K., & Ofori, E. K. (2019). Prevalence and predisposing factors of brachial plexus birth palsy in a regional hospital in Ghana: a five year retrospective study. The Pan African Medical Journal, 32. (This study looked at the prevalence and risk factors of brachial plexus birth palsy in a Ghanaian hospital. The researchers found that 14.7 percent of 320 cases involved BPBP. They also found that over 93 percent of these BPBP cases involved Erb’s palsy. The researchers concluded that the country should educate the public about BPBP’s risk factors. They also concluded that pregnant women should frequently visit their physician to ensure a safe delivery.)
- Jeevannavar, Jyoti S., Sangeeta Appannavar, and Sushma Kulkarni. “Obstetric Brachial Plexus Palsy-A Retrospective Data Analysis.” Indian Journal of Physiotherapy & Occupational Therapy 13.1 (2020). (This study looked at the characteristics and prevalence of obstetric brachial plexus palsy. The researchers found that boys were more likely to suffer from these conditions than girls, Erb’s palsy was the most commonly reported condition, right-sided brachial palsy was more prevalent than bilateral and left-sided, and that many of these deliveries did not involve an instrument.)
- Thatte, M. R., et al. “Obstetric Brachial Plexus Palsy. Diagnosis and Management Strategy.” Journal of Peripheral Nerve Surgery (Volume 1, No. 1, July 2017) 2: 9. (This study looked at obstetric brachial plexus palsy’s diagnosis and management strategies. The researchers found that obstetric brachial plexus injuries were “eminently treatable,” necessitated early referrals, required an algorithm that determined the need for surgery, and required early detection of secondary deformities. They also found that delaying surgeries yield worse outcomes and should be avoided.)
- Abzug, Joshua M., et al. “Loss of midline function in brachial plexus birth palsy patients.” Journal of Pediatric Orthopaedics 39.3 (2019): e232-e235. (This study assessed the etiology and treatment of brachial plexus birth palsy patients with midline function loss. The researchers found that BPBP patients who undergo surgery may lose midline function. They also found that derotational humeral osteotomies could restore midline function. The researchers concluded that external rotation improvement procedures should be performed to minimize midline function limitations.)
- Dzulkifli, Nurul Hafizah, Rozlin Abdul Rahman, and Noor Azliyana Azizan. “Early Physical Rehabilitation for Children with Erb’s Palsy: A Systematic Review.” International Journal of Allied Health Sciences 5.1 (2021). (This review identified early rehabilitation treatments for Erb’s palsy children. The researchers assessed 29 full-text articles. They extensively reviewed six of them. The researchers concluded that physical therapy should begin immediately after a diagnosis. They also found that combining conventional physical therapy and advanced exercises, including modified constraint-induced therapy and virtual reality, was effective. The researchers concluded that the review would help Malaysian physical therapists plan appropriate Erb’s palsy treatments based on injury level and severity.)
- Awad, Ahmed Saad, Mostafa Soliman Ali, and Mohamed Ismail Elassal. “Correlation between age, muscle architecture, and muscle strength in children with Erb’s palsy.” Bulletin of Faculty of Physical Therapy 26.1 (2021): 1-9. (This study looked at how age, muscle strength, and muscle architecture in Erb’s palsy children. The researchers evaluated 40 children with this condition. They found muscle weakness in Erb’s palsy children affected muscle architecture parameters. The researchers also found that these parameters increased with age.)
- Belabbassi, Hanene, Amina Imouloudene, and Houria Kaced. “Risk factors for obstetrical brachial plexus palsy.” Mustansiriya Medical Journal 19.1 (2020): 30. (This study looked at obstetrical brachial plexus palsy’s risk factors. The researchers found that macrosomia, labor dystocia, and instrumental vaginal deliveries were risk factors. They also found that vaginal breech delivery, parity, shoulder dystocia, and C-sections were not risk factors.)
- Abdelaziz, Ashraf M., et al. “Teres major transfer to restore external rotation of shoulder in Erb palsy patients.” Journal of Shoulder and Elbow Surgery 29.5 (2020): 941-945. (This study looked at how teres major transfers affected the infraspinatus tendon in Erb’s palsy patients. The researchers examined 20 patients. They found that teres major transfers improved shoulder abduction, active external rotation, and passive external rotation. Two cases showed internal rotation degree loss. However, the researchers found that physiotherapy resolved these issues. They concluded that teres major transfers improved Erb palsy patients’ shoulder function.)
FAQs: Erb’s Palsy
Below are simple, easy to understand answers to some of the most common questions and concerns about Erbs palsy and related conditions.
What is Erb’s palsy?Erb’s palsy is a birth injury in which damage to the brachial plexus nerves at the base of the baby’s neck occurs during vaginal delivery resulting in full or partial paralysis of the arm.
What does Erb’s palsy look like? A child with Erb’s palsy will usually have some noticeable level of paralysis or disability in one of their arms. The affected arm may be smaller, non-mobile, and sometimes twisted or contorted.
How does Erb’s palsy happen?Erb’s palsy happens when the nerves at the base of a baby’s neck are stretched out and torn during a difficult vaginal childbirth.
What nerves are damaged in Erb’s palsy?Erb’s palsy results from damage to a nerve juncture in the brachial plexus known as Erb’s point, where the C5 and C6 nerves join together to create the upper branch or trunk the brachial plexus.
What is waiter’s tip hand?Waiters tip hand is a name used to describe the common deformity resulting from Erb’s palsy where the arm hands limp with internal rotation at the elbow and wrist causing to appear as if its being held out for a tip.
Can Erb’s palsy be cured?Treatment options for Erb’s palsy vary depending on who extensive the nerve damage is. If the nerve damage is mild, Erb’s palsy will eventually go away with minimal treatment. More severe damage to the nerves can be permanent and not treatable.