Help Center
Online Resource Center for Information on Birth Injuries.
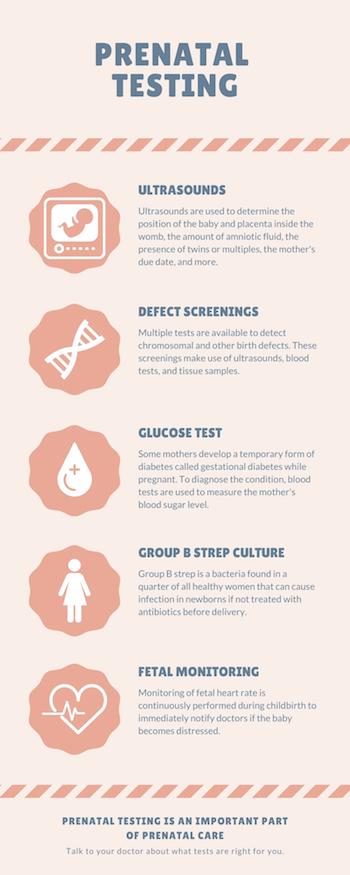
You can start getting prenatal care as soon as you know you are pregnant, or even before you become pregnant. At prenatal care visits, when you visit a doctor for check-ups during pregnancy, you may have a variety of tests done. These tests check that you and the fetus are healthy and that no birth defects or other problems exist.
Some prenatal tests will be repeated throughout pregnancy, while others happen once or a few times throughout pregnancy. Your doctor will determine what tests need to be done and when, altering this agenda throughout your pregnancy if anything changes. Mothers may need more testing or additional tests depending on their age or other risk factors.
Some tests are necessary to catch serious problems before they occur. Screenings for conditions like Down syndrome, however, are entirely optional. As with any medical procedure, it is your right to ask why the test is being done as well as its benefits and risks.
Ultrasounds are the medical test that most people associate with pregnancy. The doctor puts gel on the mother’s stomach and presses an ultrasound wand against her skin. High-frequency sound waves display an image of the fetus inside the uterus.
An ultrasound is used to check:
Ultrasounds are performed once, multiple times, or as needed. However, an ultrasound is only required if there is a medical concern. If the pregnancy is uncomplicated and the mother has no risk factors, there is not necessarily a need for an ultrasound1.
These screenings are intended to discover the probability that a fetus has a chromosomal disorder. Chromosomes are the structures found in every cell which hold genetic material. Sometimes, chromosomes are missing a part or have another abnormality.
This can happen if something goes wrong when cells are forming or if the mother was exposed to a harmful substance. Down syndrome and Edward’s syndrome are examples of chromosomal abnormalities.
These tests can also detect other problems, such as heart defects or open neural tube defects like spina bifida. Neural tube defects are problems with the formation of the brain, spinal cord, and spine. Spina bifida, for example, is when the neuron-dense spinal cord is not completely enclosed within the bones and membranes of the spine.
In a first trimester screening, ultrasound is used to examine the back of the baby’s neck and nose. A buildup of fluid or a missing nasal bone hint at the possibility of a problem. The mother’s blood is also tested. In the second trimester, a doctor performs various blood tests, checking for abnormalities in hormone and protein levels.
These tests are used to confirm genetic abnormalities and birth defects. These sorts of tests are sometimes suggested for mothers who are at risk for these issues. Women who are 35 or older, have a genetic predisposition, or who have had a child with a birth defect before may want to get this testing done. First and second trimester screenings can also show if a pregnancy is at risk for genetic abnormalities or birth defects.
Chorionic villus sampling looks at tissue from the placenta and detects conditions like Down syndrome and cystic fibrosis. In this test, doctors will insert a small tube through the cervix or a thin needle through the belly into the uterus. These methods are used to extract a bit of tissue from the placenta, which is sent to a lab for analysis.
Amniocentesis is a similar test that detects conditions like Down syndrome and spina bifida. A needle is inserted through the belly into the amniotic sac, and a sample of the fluid within is extracted for analysis.
Gestational diabetes affects some women during pregnancy. It is a temporary form of diabetes that occurs in 10% of pregnancies. Diabetes is essentially the body’s inability to correctly process sugar from food. High blood sugar can be dangerous, causing fatigue, weight loss, headaches, and possibly worse problems.
Doctors screen for gestational diabetes after about 27 weeks of pregnancy. The test involves drinking a very sugary drink and measuring the body’s response. High blood sugar an hour after consuming the drink means that the mother’s body isn’t properly processing glucose and may have gestational diabetes. If this is the case, doctors will perform a longer version of the screening in order to confirm a diagnosis.
Around the 36th week of pregnancy, doctors will look for the presence of Group B strep bacteria in the mother’s vagina and anus by taking swabs. Bacteria can potentially cause pneumonia or serious infection for the newborn after it passes through the birth canal. Urine testing is also used to check for urinary tract infections and other issues.
Group B strep is found in a quarter of all healthy women. This means testing for the bacteria is routine for all pregnant women. Those who test positive will be given antibiotics, which decreases the risk of babies developing an infection.
During childbirth, fetal monitoring is continuously performed in order to alert doctors if the baby becomes distressed. This is done using an “ultrasound transducer,” which is strapped onto the mother’s stomach to record the fetus’ heart-beat and display it on a monitor.
Fetal monitoring is also done prior to labor and delivery. It is a routine procedure at any prenatal checkup and does not mean that your baby is in danger. The doctor may listen to the fetus’ heart rate through a stethoscope or use a Doppler ultrasound device.
Late in pregnancy, doctors may perform a nonstress test, used to determine if there is a problem with the baby. If the pregnancy is high-risk or the mother suspects that something is wrong—the baby isn’t moving like normal or she is bleeding—this test may be needed.
A belt is placed around the mother’s belly which helps doctors know when the fetus is moving. They measure the fetal heart rate in response to its movements. If the fetus does not respond normally, it may indicate that the fetus is deprived of oxygen and that emergency action is needed.
A pregnancy is considered high-risk when a mother:
A pregnancy is also high-risk when issues such as these arise:
Cahill, Alison G., et al. “A prospective cohort study of fetal heart rate monitoring: deceleration area is predictive of fetal acidemia.” American Journal of Obstetrics and Gynecology 218.5 (2018): 523-e1. (This study looked at whether fetal monitoring patterns could predict acidemia. The researchers found that total deceleration areas were the best acidemia predictor.)
Nazari, Sakineh, et al. “Diagnostic value of non-stress test interpreted by smart interpretive software.” Journal of Midwifery and Reproductive Health 6.3 (2018): 1384-1389. (This study looked at smart interpretative software’s ability to accurately read non-stress tests. Based on their results, the researchers found that computers accurately read non-stress test results. This reduced false-negative and false-positive diagnoses.)
Retnakaran, Ravi, and Baiju R. Shah. “Glucose screening in pregnancy and future risk of cardiovascular disease in women: a retrospective, population-based cohort study.” The Lancet Diabetes & Endocrinology 7.5 (2019): 378-384. (This study looked at whether glucose screening tests identified cardiovascular disease risk factors in women without gestational diabetes. The researchers found that non-gestational diabetic women with abnormal glucose test results were at high risk for cardiovascular disease. They concluded that glucose screening could identify the future cardiovascular disease risk in non-gestational diabetic women.)
Salomon, L. J., et al. “Risk of miscarriage following amniocentesis or chorionic villus sampling: systematic review of literature and updated meta‐analysis.” Ultrasound in Obstetrics & Gynecology 54.4 (2019): 442-451. (This study looked at whether amniocentesis and chorionic villus sampling increased the miscarriage risk. The researchers found that the miscarriage risk following these tests was negligible compared to control groups with the same risk profile.)
Wollheim, Cláudia, et al. “Group B Streptococcus detection in pregnant women via culture and PCR methods.” Revista da Sociedade Brasileira de Medicina Tropical 50.2 (2017): 179-183. (This study looked compared the effectiveness of PCR tests versus culture tests in testing for Group B strep bacteria. The researchers found that PCR tests were “a faster and more efficient method for GBS screening” than culture tests.)