Help Center
Online Resource Center for Information on Birth Injuries.

Rh factor is a specific type of protein that most people have on the outside surface of red blood cells in their body. People who have this protein on their red blood cells are considered “Rh positive” and those without are “Rh negative.” During pregnancy a mother’s Rh factor status becomes significant because if it is different from her baby it can create a dangerous complication called Rh incompatibility. This occurs in cases where the mother is Rh negative and her baby is Rh positive.
There are 4 different human blood types: A, B, AB, and O. A person’s specific blood type is based on what kind of antigens they have on their blood cells. In addition being one of the 4 blood types, each person’s blood is either positive or negative depending on whether they have the Rh factor protein.
Rhesus (Rh) factor is a genetic protein found on the surface of red blood cells. About 85% of people have the Rh factor protein on their blood cells. These people are considered Rh positive. The remaining 15% of people do not have the Rh factor protein on their blood cells. These people are considered Rh negative.
Generally, a person’s blood type and whether they are Rh positive or negative is not significant because it has no impact on their health. However, during pregnancy a mother’s Rh factor status becomes important because it may pose some health risks to her baby. If a pregnant woman has Rh negative blood and her baby has Rh positive blood, it creates a potential complication known as Rh incompatibility. Rh factor type is a genetic baby’s inherit from their parents. Mothers who are Rh negative can have Rh positive babies if the father has Rh positive blood.
During pregnancy, Rh incompatibility is a condition which occurs when the baby’s blood has the Rh factor protein (Rh positive), but the mother’s blood does not have Rh factor (Rh negative). Rh incompatibility between mother and baby during pregnancy can be problematic and create serious risks. If the mother’s Rh negative blood mixes with the baby’s Rh positive blood, the mother’s immune system will start producing antibodies that can be very harmful to her baby.
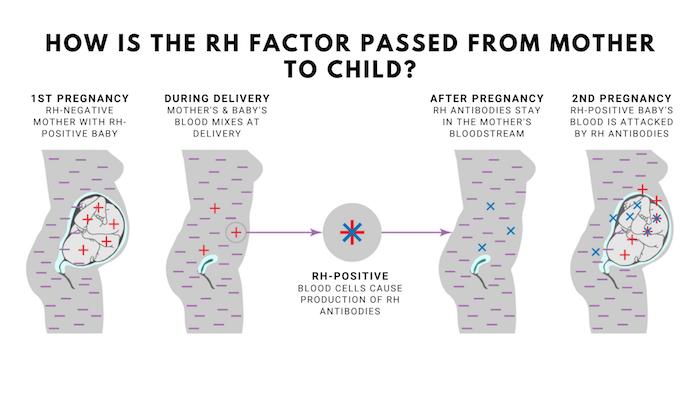
Generally, the mother and baby do not mix blood during pregnancy. However, a small amount of the baby’s blood can come in contact with the mother’s during delivery, abdominal trauma, bleeding during pregnancy, or from various prenatal diagnostic tests. If this mixing occurs and mother and baby have incompatible Rh blood types, the mother’s body will treat the Rh factor protein from the baby’s blood as a foreign invader or infection. This will trigger the mother’s immune system to create defense proteins called Rh antibodies. These Rh antibodies can cross the placenta and attack the baby’s blood. In effect, the mother’s body will act as if she is allergic to her own baby.
If the mother’s Rh antibodies attack the baby in womb they will effectively breakdown the baby’s red blood cells which could lead to life-threatening anemia. Anemia is a condition where there are not enough red blood cells to properly carry oxygen throughout the body. This condition can become severe and cause serious illness, brain damage, or death in the baby.
Rh incompatibility between mother and baby tends to be a mild problem in the first pregnancy and then gets more serious in subsequent pregnancies. This is because in the first pregnancy with Rh incompatibility the Rh antibodies produced by the mother’s immune system are not as strong or aggressive. Major problems are more likely to occur in a second or third pregnancy with Rh incompatibility because the mother’s immune system response will be more advanced and aggressive. In subsequent pregnancies the more advanced Rh antibodies produced by the mother will be more likely to cross the placenta and damage the baby’s red blood cells.
It is not all that uncommon for mother and baby to have incompatible Rh factor blood types. This blood incompatibility only becomes a problem in the event that the baby’s blood mixes with the mother’s blood. Mixing of blood between mother and baby does not normally occur during pregnancy, but there are certain events and prenatal diagnostic tests in which blood mixing is likely to occur including
When a mother’s immune system attacks the baby due to Rh factor incompatibility, it can destroy the baby’s red blood cells. This results in a condition called hemolytic anemia or hemolytic disease. Hemolytic anemia in a fetus will often cause very serious and potentially fatal health problems including:
All pregnant women should get a blood type test as part of their initial prenatal care to determine if they are Rh negative. If the blood type test confirms that the mother is Rh negative, another type of blood test called an antibody screen will be performed. The antibody screen will determine whether the Rh negative mother has already developed antibodies to Rh-positive blood that might attack her baby.
If the mother is Rh negative but she has not yet developed Rh antibodies, then doctors will normally give her Rh immunoglobulin (RhIg) injections in the hopes of preventing any Rh factor problems. RhIg injections can prevent the mother’s immune system from creating the Rh antibodies that can potentially harm her baby. RhIg injections are typically administered in the 28th or 29th week of pregnancy and then again shortly after childbirth.
RhIg is only an effective treatment option if the mother’s has no Rh antibodies. Once these antibodies are created by a mother’s immune system RhIg will not work. When these occurs doctors will closely monitor the baby during pregnancy for signs of hemolytic anemia. If severe levels of anemia develop in the baby, in utero blood transfusions may be given to replenish the baby’s damaged red blood cells. Early delivery will usually be necessary in these cases.