Help Center
Online Resource Center for Information on Birth Injuries.
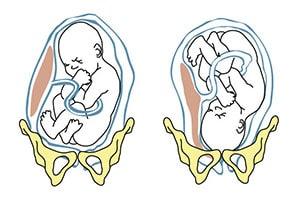
Not all babies move into the normal head-first presentation before delivery. Instead, a certain percentage of babies do not reposition and end up with their butt and/or feet downwards towards the birth canal with the head up.
This referred to as the “breech” position or breech presentation. Breech position is not normal and consider a pregnancy complication. The occurrence rate of breech position is around 5% or 1 out of every 25 babies in full-term pregnancies. The occurrence rate for breach presentation is significantly higher, however, in preterm pregnancies.
Normally in the last few weeks of a pregnancy the baby will gradually reposition itself in the head down presentation in preparation for birth. Head first is the normal presentation because it is the optimal position to safely and effectively facilitate vaginal delivery. When in the head first position the crown of the baby’s skull functions like a spear head which pushes into and through the birth canal.
Breech presentation generally includes any presentation in which the baby’s butt or feet are pointing down towards the birth canal. However, there are several different recognized subtypes of breech presentation depending on the specifics and extent of the baby’s abnormal position and the positioning of the legs:
The exact reason why breech presentation occurs is still not fully understood but numerous studies have identified a number of pregnancy conditions and/or complications that are known to increase the risk of breech presentation. The conditions which make breech presentation more likely to occur include:
The occurrence of any of these complications during pregnancy can significantly increase the chances of breech presentation occurring. However, breech presentation can occur in a normal pregnancy without complications.
Breech presentation is something that gets diagnosed towards the very end of a full term pregnancy. A formal diagnosis of breech presentation is not made until at least the 35th week of pregnancy because before week 35 it is perfectly normal for a baby to be positioned head-up or sideways. Repositioning is something that the baby is supposed to naturally do on their own in the final few weeks before birth.
Diagnosis of breech presentation will start in a prenatal examination occurring at or sometime after the 35th week of gestation. The doctor will initially perform a manual abdominal exam to gently feel around and identify the apparent position of the baby’s head, butt and feet. If the baby doesn’t seem to be in the expected position an ultrasound will usually be done to confirm the diagnosis of breech presentation. If ultrasound imaging is not enough there are also special prenatal X-rays that can be done to give doctors a more accurate image of the baby’s presentation.
When a baby is in breech position attempting a vaginal delivery can be very dangerous and most OB/GYNs will automatically plan to deliver the baby via C-section. There are several reasons why vaginal delivery of a breech baby is so hazardous.
For starters, breech presentation makes the basic mechanics of vaginal delivery much more difficult. The baby’s head is the largest part of their body so it is the most difficult to push through the birth canal. This is why brachial plexus palsy is the most common injury in a vaginal breech delivery. In a normal, head-first delivery the crown of the baby’s head sort of spears its way into and through the birth canal. Getting the head safely through the birth canal in the reverse direction is much more difficult and potentially dangerous.
Another major reason why vaginal delivery from breech position is so hazardous is because there is a much higher risk of a delivery complication called umbilical cord prolapse. Umbilical cord prolapse is one of the most dangerous events that can occur during childbirth. It occurs when the umbilical cord (the baby’s lifeline to the mother) drops down into the birth canal in front of the baby (instead of behind like in a normal delivery). When the cord goes first and the baby comes through the birth canal after the umbilical cord gets squeezed and compressed against the walls of the birth canal by the baby’s head and body. This can severely restrict or even cut off oxygen supply to the baby and cause major brain injuries or even death from perinatal asphyxia.
Attempting a vaginal delivery when the baby is in breech position can greatly increase the risk of a birth injury. Although there is currently a major push towards doing less C-sections, breech presentation is a situation where a planned C-section is simply the most sensible option. This is particularly true for premature babies that are more fragile.
Athiel, Y., et al. (2022). Association Between Hospitals’ Cesarean Delivery Rates For Breech Presentation And Their Success Rates For External Cephalic Version. European Journal of Obstetrics & Gynecology and Reproductive Biology, 270, 156-163.
This article looked at the association between a hospital’s C-section and external cephalic version rates. The researchers found that the ECV success rates correlated with C-section rates for persistent breech presentations.
Benmessaoud, I., et al. (2022). Analysis of spontaneous labor progression of breech presentation at term. PloS one, 17(3), e0262002.
This article looked at the labor progression pattern in breech presentation patients and determined whether the breech type or parity affected cervical dilation speed. The researchers found that the labor progression’s first stage in breech presentation involved latent and active phases. They also found that labor progression should be interpreted based on parity and breech type did not seem to influence the cervical dilation rate when adequately managed.
Claire, G., et al. (2022). Neonatal morbidity and mortality for preterm in breech presentation regarding the onset mode of labor. Archives of Gynecology and Obstetrics, 1-10.
This study compared the neonatal mortality and morbidity rates in preterm breech deliveries involving induced labor and spontaneous labor. The researchers found that both groups had similar neonatal mortality and morbidity rates. They concluded that the onset mode of labor did not seem to affect neonatal mortality and morbidity in breech presentation cases.
Coskun, B., et al. (2020). Comparison of Emergency and Elective Cesarean Sections in the Breech Presentation: A Case-Control Study.
This study compared outcomes in breech presentation pregnancies that underwent an emergency C-section and those that underwent an elective C-section. The researchers found that the emergency C-section group had lower Apgar scores and postoperative hemoglobin levels. They also found that cervical dilations of two centimeters and above in emergency C-sections were associated with lower hemoglobin counts, increased blood transfusion needs, and NICU transfers. The researchers concluded that healthcare providers should use caution when considering emergency C-sections and avoid iatrogenic preterm births.
Lallemant, M., et al. (2021). Asymmetric pelvis and term breech presentation: is planned vaginal delivery still a safe option? Archives of Gynecology and Obstetrics, 304, 919-927.
This study looked at whether planned vaginal deliveries were safe for term breech presentations involving asymmetric pelvises. The researchers found higher vaginal delivery rates in the asymmetric pelvis group compared to the symmetric group. They also found no statistical differences in neonatal and maternal complications. The researchers concluded that breech presentation births were “not an indication for” an elective C-section.
Gunay, T., et al. (2020). Comparison of maternal and fetal complications in pregnant women with breech presentation undergoing spontaneous or induced vaginal delivery, or cesarean delivery. Taiwanese Journal of Obstetrics and Gynecology, 59(3), 392-397.
This study compared and contrasted complications in spontaneous, induced, or C-section deliveries that involved breech presentation. The researchers found that induced vaginal deliveries had the highest complication rate, while C-sections had the lowest. They concluded that healthcare providers should consider specific delivery types’ risks and benefits when handling breech presentation pregnancies.
Martel-Santiago, C.R., et al. (2020). Delivery in breech presentation: Perinatal outcome and neurodevelopmental evaluation at 18 months of life. European Journal of Obstetrics & Gynecology and Reproductive Biology, 255, 147-153.
This study compared the outcomes of cephalic and breech deliveries. The researchers found that C-sections involving breech presentations had lower Apgar scores than cephalic presentations. They also found that vaginal concluded that healthcare providers should implement specific protocols in certain breech presentation pregnancies to achieve similar outcomes as cephalic presentation ones.
Toijonen, A.E., et al. (2020). A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case-control study. Archives of Gynecology and Obstetrics, 301, 393-403.
This study looked at whether breech presentation’s common risks in term labor were present in preterm labor. The researchers found that breech presentation-associated factors in preterm breech deliveries were similar to factors in term pregnancies. By contrast, they found that exceptionally preterm breech births had comparable risks to cephalic presentations.